
Cancer has long been gaining ground as the leading cause of death in the United States for people under the age of 85. Since peaking in the mid 1960s, heart disease rates have fallen, while cancer has continued to steadily climb. For years there have been studies that have tried to determine the relationship between allergies and cancer. Some research has shown an inverse relationship between allergies and cancer, meaning allergies actually INHIBIT cancer growth rates, while other studies have shown the exact opposite of this. So which study is correct? We’re going to take a look at research through the years, and try to help sort out the convoluted link between allergies and cancer.
The Link Between Allergies and Cancer
Is there a connection between cancer and allergies? Simply put, yes. On the most basic level, the basis for this connection is the immune system, which is our body’s self-defense system. The immune system includes many different kinds of specialized cells which protect us from diseases by killing foreign invaders like bacteria and parasites. As we know with allergies, the immune system sometimes picks up on false positives and identifies normally-harmless substances like pet dander, pollen, and dust mites, as threats.
 In the case of allergies, the immune system becomes hypersensitive to substances that are normally harmless, and immune cells overreact to that substance, causing inflammation and allergy symptoms. On the other hand, in the case of cancer, the immune system often under reacts. After all, cancer cells are nothing more than normal cells with damaged DNA. Think of these two instances in terms of a type of warfare. With allergies, our soldiers identify those trees at the edge of the battlefront as a threat. They rouse the other troops, prepare the defenses and launch an all out assault on the trees. With cancer, our soldiers see a fellow troop and recognize him as on our side. The troop could be teeming with the plague, but since they have on the right uniform, we do not perceive a threat, even though it could be infecting the rest of the troops.
In the case of allergies, the immune system becomes hypersensitive to substances that are normally harmless, and immune cells overreact to that substance, causing inflammation and allergy symptoms. On the other hand, in the case of cancer, the immune system often under reacts. After all, cancer cells are nothing more than normal cells with damaged DNA. Think of these two instances in terms of a type of warfare. With allergies, our soldiers identify those trees at the edge of the battlefront as a threat. They rouse the other troops, prepare the defenses and launch an all out assault on the trees. With cancer, our soldiers see a fellow troop and recognize him as on our side. The troop could be teeming with the plague, but since they have on the right uniform, we do not perceive a threat, even though it could be infecting the rest of the troops.
Since allergic conditions spur the immune system into action, do allergy sufferers have less risk of developing cancer? Over the past few years, scientists have been researching that exact question.
Allergy and Cancer Risk – The Good
 A “balanced polymorphism” is a genetic pattern that can offer protection against certain diseases while increasing the risk of others. For example, carriers of sickle-cell anemia are resistant to malaria. Similarly, allergies may protect people against certain forms of cancer.
A “balanced polymorphism” is a genetic pattern that can offer protection against certain diseases while increasing the risk of others. For example, carriers of sickle-cell anemia are resistant to malaria. Similarly, allergies may protect people against certain forms of cancer.
A 2005 article in the journal Cancer Research suggests that allergies and asthma reduce the risk of developing brain cancer. (So there’s at least one good thing about having allergies!)
Another 2005 article in the American Journal of Epidemiology suggests an inverse association between a history of allergy and cancer mortality, which means that allergies may offer some protection against cancer in general, but the strength of the evidence is limited.
A more recent study, a 2013 article in the American Journal of Epidemiology looks at the association between allergies and cancer. Associations between self-reported allergies and various cancers have been investigated in a number of epidemiologic studies (1–3); reduced risk for pancreatic cancer is among the most consistent findings. A meta-analysis of 14 pancreatic cancer studies showed a 30% reduced risk in those with any allergies and a 45% reduced risk in those with respiratory allergies such as hay fever in studies with direct interviews rather than proxies (4).
In a 2008 meta analysis of studies and research on this topic, the National Institute of Health found that some of the most common inverse relationships (read allergies = lower risk of cancer) were “associated with cancers of tissues that interface with the external environment.”
These studies, and others, all seem to point to a somewhat positive relationship between certain types of allergies and cancer. Unfortunately, the relationship between these two things is not as clear cut as first appearances may indicate.
Allergy and Cancer Risk – The Bad
Not all studies show that allergies can reduce the risk of cancer. A 1992 article that appeared in the American Journal of Epidemiology found that males with drug allergies had a 33% increase in the risk of getting cancer; in contrast, females with drug allergies showed a 21% decrease in the risk of getting cancer. The study also showed that a history of allergies seems to increase the risk of prostate cancer and breast cancer, but decreases the risk of ovarian cancer. Moreover, a 2004 article in the journal BMC Public Health suggests that people who have asthma and eczema are more likely to develop cancers of the blood.
 If we continue to examine even more recent research, the findings only seem to reinforce the negative relationship between allergies and cancer.
If we continue to examine even more recent research, the findings only seem to reinforce the negative relationship between allergies and cancer.
A 2003 study published in the American Journal of Hematology shows a link between certain types of hematologic malignancies (cancers of the blood) and allergies, but the link was only found in women. This association was deemed a moderate risk for those that are allergic to plants, grass, or trees.
Another study published in March of 2015 in the Journal of Leukocyte Biology focused on allergies and more specifically breast cancer in women. By inducing pulmonary inflammation (the same variety you would see with allergies), researchers were able to demonstrate higher rates of metastasis. Changes in the pulmonary microenvironment (inflammation) allowed cancer to grow and spread more quickly throughout the body.
The results of these studies suggest that, while a history of allergies may offer some protection against certain types of cancer, the relationship between allergies and cancer is complex—the relationship depends on the specific type of allergy and the specific type of cancer.
Inflammation, Allergies and Cancer
 Allergic diseases appear to reduce the risk of cancer in some cases, perhaps by keeping the immune system on its toes, so to speak; but too much stimulation of the immune system (too much inflammation) can damage the body and increase the risk of cancer.
Allergic diseases appear to reduce the risk of cancer in some cases, perhaps by keeping the immune system on its toes, so to speak; but too much stimulation of the immune system (too much inflammation) can damage the body and increase the risk of cancer.
A 2007 paper published in the journal Cell describes what could be the long-elusive mechanism through which inflammation can promote cancer.
“Although there is plenty of evidence that chronic inflammation can promote cancer, the cause of this relationship is not understood,” says Alexander Hoffmann, an assistant professor of chemistry and biochemistry at U.C. San Diego, who led the study. “We have identified a basic cellular mechanism that we think may be linking chronic inflammation and cancer.”
A protein called p100 allows for the communication between the inflammation and development processes. Some amount of dialogue is beneficial, but too much dialogue (which results from chronic inflammation) can lead to unrestrained development (cancer).
“Studies with animals have shown that a little inflammation is necessary for the normal development of the immune system and other organ systems,” explains Hoffmann. “We discovered that the protein p100 provides the cell with a way in which inflammation can influence development. But there can be too much of a good thing. In the case of chronic inflammation, the presence of too much p100 may over-activate the developmental pathway, resulting in cancer.”
More recently, a study published in 2014 delineates the link between cancer and histamines. They found that histamines actually play a vital role in protecting tumors from the immune system, and that “by blocking the production of histamine in animal models, the researchers were able to interrupt a process that promotes melanoma growth.” Histamines activate suppressor cells which aid in the growth of tumors by suppressing the immune system.
These two novel studies get down to the nuts and bolts of what is driving allergies and cancer, and more importantly, they also shed some light on potential ways to combat cancer.
Immunotherapy: Different Applications for Allergy & Cancer
Immunotherapy for allergy sufferers is commonly referred to as allergy shots. And now sublingual immunotherapy allergy drops are available as well. Allergy shots are made up of the allergen(s) that cause the allergic reaction. The amount of the injected allergen gradually increases over a long period of time, usually at least two years. Immunotherapy helps the immune system build up a tolerance to the specific allergens so that immune cells do not overreact when they are exposed to the allergen(s).
 Immunotherapy for cancer patients has a much different goal; its effect is nearly the opposite, in fact. The goal of cancer immunotherapy is to somehow “tag” the cancer cells so that the immune system knows to attack them. Allergy immunotherapy attempts to calm the overreacting immune cells, whereas cancer immunotherapy attempts to spur sluggish immune cells into action. Think back to the warfare analogy at the beginning of this article to help you understand this..
Immunotherapy for cancer patients has a much different goal; its effect is nearly the opposite, in fact. The goal of cancer immunotherapy is to somehow “tag” the cancer cells so that the immune system knows to attack them. Allergy immunotherapy attempts to calm the overreacting immune cells, whereas cancer immunotherapy attempts to spur sluggish immune cells into action. Think back to the warfare analogy at the beginning of this article to help you understand this..
BCG immunotherapy is often used to treat bladder cancer. BCG is a solution of genetically engineered tuberculosis (TB) bacteria that’s used as a TB vaccine in some countries. In the cancer treatment, the BCG is administered directly into the bladder via catheter, and the BCG elicits an immune system response. This response activates the immune system’s killer cells, and they attack the cancerous cells. For some reason, the immune system’s response seems to target the cancer cells (as opposed to chemotherapy, for example, which also kills all surrounding healthy cells), perhaps because the BCG has an affinity for the cancer cells and somehow attaches to them. Thus, TB bacteria can be used to “tag” cancer cells.
Revolutionary Allergy Vaccines in Development
Ironically, scientists at Cytos Biotechnology in Zurich are working on an allergy vaccine that also uses genetic material from the TB bug. The harmless DNA tricks the immune system into thinking it is being attacked by a foreign invader, so the disease-fighting white blood cells rush into action. This immune response provides protection against allergic responses. The vaccine is still in the early stages of development, but in the vaccine’s most recent trial, 40 adults that are allergic to dust mites were given either weekly vaccine shots or a placebo “dummy” shots for six weeks. Those that were given the real shots quickly became tolerant to dust mite allergen, some being 100 times more resistant.
More recently, Circassia has been working on a similar approach—an allergy vaccine, more specifically, a cat allergy vaccine. After multiple clinical trials, the ToleroMune T-cell vaccine is in the final stage of clinical testing. “Regulatory T cells inhibit mast cells, stopping histamine from being released and thereby effectively blocking the inflammatory cascade that leads to the early-phase allergic response.” Unlike other types of immunotherapy, this approach acts quickly, reducing allergic response by over 50% after just four treatments, and subsequent trials have shown that the results of the treatment appear to be long lasting. This specific topic and vaccine are ones we’ve mentioned several times in our blog throughout the years, due to the promise it shows in combating allergies.
From the 2014 article mentioned at the end of the last segment, researchers were able to show that the suppressor cells that shielded tumors and allowed them to grow could potentially be decreased by something as common as an over-the-counter antihistamine. On this side of the coin, they are again looking at histamines and the role they play, but in cancer cell/tumor growth.
Environmental Control of Allergens & Carcinogens
 Besides the immune system, there’s another big connection between allergies and cancer: You can guard against both allergies and cancer by practicing environmental control. Allergens trigger allergic reactions, and carcinogens cause cancer; you can decrease your risk of developing diseases by keeping allergens and carcinogens out of your environment.
Besides the immune system, there’s another big connection between allergies and cancer: You can guard against both allergies and cancer by practicing environmental control. Allergens trigger allergic reactions, and carcinogens cause cancer; you can decrease your risk of developing diseases by keeping allergens and carcinogens out of your environment.
Throughout our site, there are countless articles about how you can better manage your indoor environment and how to control and limit your exposure to allergens, so we will not spend time on them here. Instead, we will now turn our attention to carcinogens.
What is a Carcinogen?
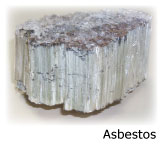
Do you remember when we noted how a cancer cell is simply a normal cell with damaged DNA? Simply put, a carcinogen is a substance that damages DNA and promotes cancer. Some natural substances can be carcinogens, like asbestos, ultraviolet radiation (UV) in sunlight, x-rays, gamma radiation and Aflatoxin B1, which is a toxin produced by a fungus that grows on stored grains, nuts, and peanut butter. Some viruses, such as Hepatitis B and the human papilloma virus (HPV), have also been shown to cause cancer.
![]() Common man-made carcinogens include various forms of air pollution like tobacco smoke and certain chemical fumes. You can reduce your risk of cancer by keeping your lungs free of carcinogens with a HEPA air purifier and HEPA mask. While a HEPA filter is always a good start, some carcinogens pass right through this type of filter. In many circumstances you will need a combination HEPA and activated carbon filter to protect you from smoke and chemical fumes. Carbon filters target compounds like smoke, chemical vapors, and fumes, trapping their molecular components by bonding with them, adhering them to the carbon and removing them from the air. Whether it is a mask or an air purifier, there are options available in both that have particle filtration (HEPA or HEPA style) and carbon filter media.
Common man-made carcinogens include various forms of air pollution like tobacco smoke and certain chemical fumes. You can reduce your risk of cancer by keeping your lungs free of carcinogens with a HEPA air purifier and HEPA mask. While a HEPA filter is always a good start, some carcinogens pass right through this type of filter. In many circumstances you will need a combination HEPA and activated carbon filter to protect you from smoke and chemical fumes. Carbon filters target compounds like smoke, chemical vapors, and fumes, trapping their molecular components by bonding with them, adhering them to the carbon and removing them from the air. Whether it is a mask or an air purifier, there are options available in both that have particle filtration (HEPA or HEPA style) and carbon filter media.
Other man-made carcinogens include formaldehyde (used to make plastics) and vinyl chloride (used to make PVC). Dr. Jospeh Mercola reports that bisphenol A (BPA), an estrogen-like compound widely used in plastic products, is associated with cancer and reproductive disorders. In one study, 95% of the people that were tested had BPA levels that could be dangerous. BPA leeches into food from plastic containers, so to be safe, you should use plastic that is BPA free.
 To reduce your exposure to BPA and other chemicals in plastic, Dr. Mercola gives the following advice: use only glass baby bottles, dishes, and cups, buy fabric toys instead of plastic ones, store food in glass containers, don’t microwave plastic, avoid canned foods, don’t use plastic wrap, and avoid water in plastic bottles. This is another topic that we have written about extensively on our blog as the research around BPA grows, and regulations regarding BPA in products, specifically baby products, form and change over time.
To reduce your exposure to BPA and other chemicals in plastic, Dr. Mercola gives the following advice: use only glass baby bottles, dishes, and cups, buy fabric toys instead of plastic ones, store food in glass containers, don’t microwave plastic, avoid canned foods, don’t use plastic wrap, and avoid water in plastic bottles. This is another topic that we have written about extensively on our blog as the research around BPA grows, and regulations regarding BPA in products, specifically baby products, form and change over time.
You probably even have carcinogens in your antiperspirant deodorant. Aluminum-based ingredients and parabens may mimic estrogen and increase the risk of cancer. Cancer researcher Philippa Darbre, PhD, of the University of Reading, says evidence is mounting that the aluminum-based active ingredient in antiperspirants can mimic estrogen in the body. “Lifetime exposure to estrogen is the risk factor which is tied most strongly to breast cancer,” says Dr. Darbre. The topic of aluminum, particularly with regard to Alzheimer’s, remains an unsettled matter and the research has yet to find consensus. Some studies show a link while others show even exposure to high levels of aluminum does not correlate to an increased risk of Alzheimer’s.
To be on the safe side, avoid all known carcinogens and suspected carcinogens whenever possible.
Cancer Prevention: Healthy Lifestyle Choices
You can also decrease your cancer risk by making healthy choices in your everyday life. Medical experts report that two-thirds of all cancers are preventable; that is, they’re related to tobacco use, excess weight, poor diet, and lack of exercise. In fact, the University of Texas MD Anderson Cancer Center reports that only five to ten percent of cancers are truly hereditary.
Smoking is the most preventable cause of cancer—smoking is responsible for 87% of all lung cancer cases and 30% of all cancer deaths. Alcohol consumption also increases the risk of getting cancer, too. While some studies show that moderate alcohol consumption may be good for the heart, alcohol is linked to cancers of the colon, breast, and liver. In terms of diet, sugar feeds cancer, so you should avoid sugar whenever possible, particularly refined sugars. Also, it is important to eat plenty of fresh fruits and vegetables and make sure that you’re getting enough omega-3 fatty acids from natural sources or supplements.
Poor sleep habits and high stress levels weaken your immune system and may increase the risk of cancer.
Finally, you should avoid getting sunburned, but you should not avoid sunlight altogether! In recent years, there has been much confusion about the role that sun plays in causing cancer. Sunlight is the source of life—it’s good for you, but not in excess. Exposure to sunlight produces vitamin D in the body, and evidence suggests that low vitamin D levels may contribute to the development of cancer. Make sure you always wear sunscreen when you are outside to avoid getting sunburned.
Cancer and allergies are both modern diseases that continue to increase in prevalence, but you can go a long way in keeping yourself healthy by taking care of yourself, enhancing your immune system with a healthy diet and exercise, and avoiding harmful substances in your environment.
